In this article, we analyze the Health Services Pack IVDR impact and its role in shaping future health regulations.
On 16 December 2025, the European Commission published a proposal to amend the EU Medical Devices Regulation (MDR) and the In Vitro Diagnostic Regulation (IVDR) with targeted measures intended to reduce regulatory complexity, cost, and unpredictability while maintaining high safety standards.
This article focuses on IVDs under IVDR and the combined-study interface (drug–diagnostic and multi-legislation studies). It explains what the proposal says today, what it could change in practice, and how different stakeholders can prepare. It also recognizes that the text is still a proposal and may change during the ordinary legislative procedure in the European Parliament and Council.
Executive summary
What matters most for IVDR stakeholders.
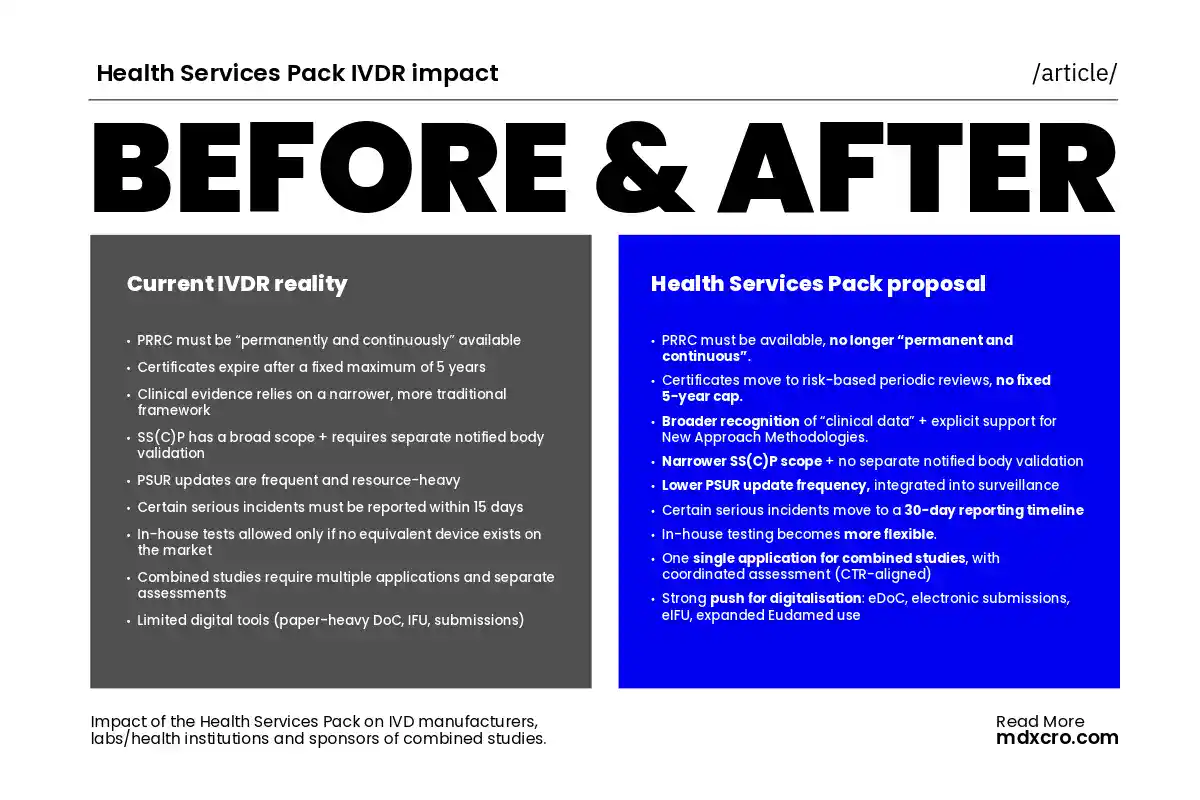
If adopted largely as proposed, the package could materially affect how IVD stakeholders plan certification lifecycles, evidence generation, post-market obligations, in-house testing, and combined-study authorisations:
- PRRC organisational burden would ease for SMEs relying on external PRRC support (availability requirement would soften; detailed qualification rules would be removed).
- Certificate validity would shift from a fixed 5-year maximum to risk-based periodic reviews during the certificate lifecycle.
- The proposal would support a broader evidence toolbox, including wider “clinical data” recognition and explicit promotion of New Approach Methodologies (including in silico testing).
- Administrative burden would reduce via a narrower scope for summary documents and lower PSUR update frequency, plus longer timelines for certain vigilance reporting.
- In-house testing under IVDR Article 5(5) would become more flexible, including (under IVDR) removing the “no equivalent device on the market” condition and explicitly bringing certain central laboratories supporting clinical trials into scope.
- For combined studies, sponsors could submit a single application triggering a coordinated assessment aligned with the Clinical Trials Regulation framework.
- Digitalisation would expand: digital EU Declarations of Conformity, more electronic submission, and electronic IFU for near-patient tests (among other measures).
The Commission frames these changes as a way to keep safety standards high while improving predictability, competitiveness, and innovation support; it cites €3–5 billion/year in cost savings at conservative estimates.
Key regulatory updates
PRRC flexibility for SMEs
Risk-based certificate validity
Broader clinical evidence
Reduced administrative burden
Flexible in-house testing (IVDR)
Streamlined combined studies
Expanded digitalisation
1) Context: why the Commission proposed a targeted IVDR/MDR revision
The Commission’s Q&A states that evaluation work identified shortcomings that negatively affect competitiveness, innovation, and patient care—pointing to inefficient coordination, divergent application of requirements, and procedures that are overly complex and costly.
The Commission describes the reform’s core objectives as:
- Reduced administrative burden and stronger coordination
- More proportionate requirements, especially for lower/medium risk devices and small patient populations
- Support for innovation, including early expert advice and regulatory sandboxes
- Greater predictability and cost-efficiency of certification, including enabling real-world evidence
- Increased digitalisation across compliance tools and conformity assessment procedures
For IVDR stakeholders, the significance is not only the “what” but also the “how”: the proposal aims to make the system more predictable and less duplicative while leveraging EU-level expertise (including expert panels and EMA support).
2) Understanding Health Services Pack IVDR Impact: what it means for IVD manufacturers
2.1 PRRC: reduced organisational friction (especially for SMEs)
The proposal would:
Remove detailed qualification requirements for the Person Responsible for Regulatory Compliance (PRRC), and
Remove the requirement that SMEs using an external PRRC must have the PRRC “permanently and continuously” available; the PRRC would need to be available (without the “permanently and continuously” standard).
Why it matters: This could reduce structural overhead for smaller IVD manufacturers and for non-EU manufacturers using EU-based regulatory operating models. It may also reshape how manufacturers design PRRC coverage (internal vs external, shared services, outsourcing structures).
2.2 Certificates: from 5-year re-certification to risk-based periodic review
The proposal would remove the current maximum 5-year certificate validity and replace it with periodic reviews proportionate to device risk during the certificate’s validity period.
In addition, the proposal’s summary of certification changes includes:
- Reduced systematic technical documentation assessment during surveillance activities (as summarised for certain IVD classes),
- The ability for notified bodies to replace on-site audits with remote audits, and
- Surveillance audits “only every two years” where justified by the absence of safety issues, plus unannounced audits “for-cause”.
Why it matters:
This is a structural shift in compliance planning—from a calendar-driven re-certification event to an ongoing lifecycle model that could be more data-driven. IVD manufacturers will likely need stronger “always audit-ready” systems and clearer change-control strategies.
2.3 Evidence toolbox: broader clinical data concepts and explicit support for in silico approaches
The proposal summarises multiple evidence-related changes, including:
- A wider range of data qualifying as clinical data,
- More flexible conditions for relying on clinical data from an equivalent device, and
- Promotion of New Approach Methodologies such as in silico testing.
Why it matters for IVDs:
IVDR evidence expectations are often the pacing item for certification and market access—particularly for novel biomarkers, decentralised testing, and CDx. A broader toolbox could let manufacturers structure performance evaluation more efficiently, but it also puts more emphasis on robust justification: the proposal supports flexibility, not a “free pass.”
2.4 Summary documents and PSUR: targeted burden reduction
The proposal would:
- Reduce the scope of devices that must have a summary of safety and (clinical) performance (SS(C)P) to those where the notified body must conduct technical documentation assessment—and remove the need for separate notified body validation of the draft summary.
- Reduce the required PSUR update frequency, with notified body PSUR review integrated into surveillance.
For IVDR specifically, the proposal text also states that:
- Manufacturers of class C and D devices would update the PSUR in the first year after the certificate is issued and every two years thereafter (or earlier in defined change situations).
Why it matters:
This change could reduce recurring workload—yet it will likely increase expectations that PSUR content is meaningful, well-argued, and operationally integrated into surveillance interactions.
2.5 Vigilance and cybersecurity: longer timelines for certain incidents, plus cyber reporting alignment
The proposal would extend the reporting timeline for certain serious incidents (those not linked to public health threats, death, or serious deterioration) to 30 days instead of 15.
It would also introduce a cybersecurity linkage:
- Certain MDR/IVDR vigilance reports that also qualify as actively exploited vulnerabilities or severe incidents under the cyberresilience framework would be made available to national CSIRTs and ENISA; and
- Manufacturers would have to report actively exploited vulnerabilities and severe incidents that do not qualify as “serious incidents” under MDR/IVDR to CSIRTs and ENISA through Eudamed;
- Cybersecurity would be explicitly mentioned in Annex I general safety and performance requirements.
Why it matters for IVD manufacturers:
Cybersecurity is not only an “IT topic.” It increasingly affects performance, safety, vigilance, and field actions—especially for connected IVD instruments, software-driven diagnostics, and laboratory information system integration.
2.6 Digitalisation: eDoC, electronic submissions, eIFU for near-patient tests, and online sales information
The proposal includes:
- Digital EU Declarations of Conformity,
- More electronic submission of MDR/IVDR information,
- Economic operators providing digital contacts in Eudamed,
- Digital technical documentation and conformity assessment documentation, and
- For IVDs, the ability for manufacturers of near-patient tests to provide electronic instructions for use.
It also introduces online-sales transparency requirements: essential device identification information and IFU information must be provided for online sales.
Why it matters:
This points toward a compliance ecosystem where document control, traceability, and market surveillance become more data-centric. Manufacturers will need disciplined digital governance to prevent inconsistency across channels.
3) What the proposal could change for labs and health institutions (IVDR Article 5(5) in-house)
The proposal would make in-house conditions more flexible, including:
- Allowing the transfer of in-house devices when justified by patient safety or public health interests, and
- Under IVDR, removing the condition that no equivalent device exists on the market.
It also explicitly adds central laboratories manufacturing and using tests exclusively for clinical trials into the scope of the in-house device exemption.
Why Health Services Pack IVDR matters
If adopted, this could significantly affect:
- The role of hospital laboratories in innovation and continuity-of-care testing,
- How health systems respond to unmet needs, niche populations, and rapidly evolving clinical practice, and
- The operational models used to support clinical trials (including biomarker-driven trials and decentralised sample workflows).
What labs should plan
Recognising the proposal may change
- Governance and documentation systems that can withstand scrutiny as “in-house” use expands in scope and visibility.
- Contracting and quality interfaces between health institutions, trial sponsors, and central labs—especially where a lab’s “in-house” position interacts with trial requirements and sponsor expectations.
4) What the proposal could change for sponsors of combined studies (drug–diagnostic interface)
4.1 A single application with coordinated assessment (CTR-aligned pathway)
For combined studies involving medicinal products, medical devices, and/or IVDs, the proposal states that a sponsor may submit a single application triggering a coordinated assessment in accordance with the Clinical Trials Regulation (CTR), noting alignment with amendments anticipated via the Biotech Act.
Why it matters:
Sponsors running biomarker-driven programmes often experience friction at the interface between medicinal product trial authorisation processes and IVDR performance study requirements. A coordinated model—if implemented in a practical, predictable way—could materially improve planning across Member States.
4.2 Performance study burden reduction in defined scenarios
The proposal also states that:
- Performance studies involving only routine blood draws would not require prior authorisation; and
- Notification of performance studies on companion diagnostics using left-over specimens would be removed.
Why it matters:
This could affect study-start timelines, especially in multi-country settings where administrative sequencing often drives critical path. For sponsors, it may also change how they design sample strategies, feasibility, and site activation planning.
5) Practical implications of Health Services Pack IVDR Impact: how stakeholders can prepare while the text remains a proposal
Because the proposal may change during negotiations, stakeholders should avoid “over-implementing” assumptions. At the same time, most organisations can act now in ways that remain valuable under multiple legislative outcomes.
5.1 For IVD manufacturers (RA/QA and clinical/performance teams)
Focus now on “no-regret” preparedness:
- Map your portfolio to where the proposal signals the biggest change: certificate lifecycle management, audit model (remote/on-site), and surveillance cadence.
- Re-evaluate your evidence strategy so it can flex across clinical studies, literature, equivalence, and (where applicable) in silico methodologies—while keeping scientific validity and traceability strong.
- Strengthen change control to align with the proposal’s intent to distinguish changes that require different levels of notified body interaction (including predetermined change control planning).
- Upgrade vigilance and cybersecurity workflows so reporting pathways align with both vigilance obligations and the proposed cyber reporting linkages (CSIRTs/ENISA/Eudamed).
- Digitise with discipline: ensure eDoC, digital IFU strategies, and online-sales content controls remain consistent and auditable.
5.2 For labs and health institutions
- Review how in-house governance could evolve if the “no equivalent device” condition disappears and trial-supporting central labs fall clearly within scope.
- Align in-house test lifecycle controls with quality expectations likely to increase as in-house scope expands in visibility and operational relevance.
5.3 For sponsors of combined studies
- Build study-start strategies around the proposal’s direction of travel: a coordinated route for combined studies and reduced administrative hurdles for defined performance study scenarios.
- Stress-test protocols for evidence coherence: regulators will still expect sponsor claims and IVD performance claims to align, even if administrative routes simplify.
6) Health Services Pack IVDR Impact and its potential global reach: what this could mean outside Europe
The Commission positions the EU as a global leader in medical device regulation and indicates the reform aims to make the sector more competitive globally.
It also explicitly links the proposal to reinforcing international cooperation, including participation in high-standard international cooperation and information-sharing mechanisms with reliable partners and strengthened uptake of international guidance.
For global manufacturers, that matters because EU compliance strategies often influence:
- Global clinical evidence planning and dossier structuring, and
- How manufacturers operationalise post-market surveillance and cybersecurity controls across regions.
(How much convergence happens in practice will depend on implementation and on how reliance mechanisms are used over time.)
FAQs
No. The Commission published a proposal on 16 December 2025. The text must go through the ordinary legislative procedure in the European Parliament and Council before any final legal changes take effect.
The proposal would remove the maximum 5-year certificate validity and replace it with risk-based periodic reviews while the certificate remains valid.
Yes. The proposal would reduce PSUR update frequency and integrate notified body PSUR review into surveillance. It also states class C and D PSUR updates would occur in the first year after certification and every two years thereafter (or earlier in defined cases).
Yes. For serious incidents not related to public health threats, death, or serious deterioration, the proposal would extend reporting timelines to 30 days instead of 15.
Yes. The proposal would make in-house conditions more flexible and, under IVDR, would remove the condition requiring “no equivalent device on the market.” It would also add certain central laboratories supporting clinical trials into scope.
The proposal states that sponsors could submit a single application for combined studies, triggering a coordinated assessment aligned with the Clinical Trials Regulation framework.
How can MDx CRO help you navigate Health Services Pack IVDR Impact effectively?
If you manufacture IVDs, run laboratory services, or sponsor combined studies, you will likely need to translate the proposal into:
- A portfolio-level impact assessment (technical documentation, evidence strategy, and certification lifecycle planning), and
- An operational plan for performance studies and combined-study submissions that remains robust even if the final text changes.
MDx CRO supports IVD manufacturers and sponsors across IVDR technical documentation, performance evaluation strategy, and combined study operational delivery (clinical operations + RA/QA alignment). The most effective next step is usually a short, structured gap-and-opportunity review tied to your portfolio and pipeline.
Need support?
We can assist you translating the Health Services Pack proposal into practical IVDR actions for your portfolio, studies, or lab activities.







