On 21 October 2025, the Council of Ministers approved Spain’s new Royal Decree for in vitro diagnostic devices. AEMPS confirmed the approval and explained that the decree complements IVDR (EU) 2017/746, strengthens patient protection, and adds national rules on language, in-house manufacturing, performance studies, and vigilance. This development anchors the Spanish IVD Regulation 2025 and sets clear obligations for manufacturers, sponsors, and laboratories. (Official announcement: AEMPS)
Spanish IVD Regulation 2025: What Changed and Why It Matters
The Spanish IVD Regulation 2025 replaces Royal Decree 1662/2000. It clarifies how IVDR applies in Spain and fills Member-State choices, including competent authority, language regime, Article 5(5) in-house devices, genetic testing and counseling, a national marketing register, performance study authorization, and vigilance and market control.
The regulation aims to raise quality, ensure traceability, and speed up corrective actions. It also improves access to certain self-tests through pharmacy channels.
Quick Guide for Busy Teams (Manufacturers, Sponsors, Labs)
- Confirm what the Spanish IVD Regulation 2025 changes for your role.
- Map licensing, registration, language, Article 5(5), ISO 15189, performance studies, and vigilance to owners and deadlines.
- Prepare Spanish-language materials and set up traceability and incident reporting workflows.
- Labs should plan ISO 15189 and Article 5(5) notifications to AEMPS.
Competent Authority and Language Rules under the Spanish IVD Regulation 2025
AEMPS is the competent authority for IVDs in Spain. Under the Spanish IVD Regulation 2025, user-facing materials for devices marketed in Spain must appear in Spanish. That includes labels, IFU, and safety notices. Regulatory submissions to AEMPS should include Spanish content. Co-official languages may be added, but Spanish is mandatory.
Action: Audit labeling, IFU, FSNs, PMS templates, and performance study files. Plan translations and version control.
Facility Licensing: Manufacturers, Sterilizers, and Importers
The Spanish IVD Regulation 2025 requires operating licenses for manufacturers, sterilizers, and importers before they place devices on the market. AEMPS evaluates facilities, personnel, and quality systems.
Each site must appoint a Technical Responsible Person (national role) and meet IVDR oversight led by a PRRC. One qualified person can cover both if they meet the criteria.
Transitional rule: Existing third-party manufacturers get up to one year from entry into force to secure the new license. Existing licenses remain valid until renewal or change, which then follow the new procedure.
Action: Confirm license status, designate the responsible person, and prepare for renewal under the new framework.
Marketing Register and Traceability
The decree creates a Spanish marketing register for devices placed on the market. Manufacturers, authorized representatives, and importers must notify product information to support traceability and market surveillance. The register complements EUDAMED and UDI.
Transitional rule: Spain will activate notifications when the register is operational. Until then, use existing national channels.
Action: Build a clean data set for device identifiers, certificates, and supply chains. Prepare to submit once AEMPS opens the register.
In-House Devices (Article 5(5) IVDR): What Labs Must Do Now
Scope and intent
The Spanish IVD Regulation 2025 regulates in-house IVDs made and used within the same health institution. Labs must justify need: a commercial CE-marked device cannot meet the specific clinical need. No industrial-scale production. No commercial supply to third parties.
Quality and documentation
In-house devices must meet IVDR GSPRs. Labs should keep a technical file (intended purpose, risk management, analytical and clinical performance, V&V, SOPs, and labeling for internal use).
ISO 15189 accreditation
Labs that manufacture in-house devices must obtain ISO 15189 accreditation for the manufacturing scope. Spain ties this to the transitional schedule.
Notification to AEMPS
Before starting in-house manufacture, labs must notify AEMPS and submit the Article 5(5) declaration. They must designate a responsible person for the in-house manufacturing process.
Action for labs: Launch ISO 15189 projects, finalize Article 5(5) templates, and prepare the AEMPS notification package.
Genetic Testing: Information and Counseling
The Spanish IVD Regulation 2025 requires clear information and appropriate counseling for genetic testing. Health professionals must explain limits, implications, and result interpretation. This duty applies before and after testing.
Health professionals and centers must obtain explicit informed consent from individuals before performing a genetic test. The patient must be made aware of the nature and purpose of the test and consent in writing (except where law may exempt certain public health screening). This goes beyond standard consent, recognizing the personal and familial implications of genetic data.
Before the test, patients should be informed about what the test can and cannot tell them, and after the test, a qualified professional should explain the results and any recommended follow-up. This requirement ensures genetic tests (such as those for hereditary disease risk) are not delivered without context or support, helping patients make informed decisions.
These obligations apply to genetic IVDs regardless of whether they are done in-house or as commercial tests. For example, a direct-to-consumer genetic test kit (if allowed on the market) would need to be accompanied by processes that ensure the purchaser gets necessary information and counseling. However, most genetic tests are administered in clinical settings; the decree effectively standardizes the practice of genetic counseling as part of testing.
Action: Update consent forms, patient information sheets, and SOPs for genetic counseling, including training for staff.
Performance Studies in Spain
All performance studies in Spain must first obtain a favorable opinion from an accredited Research Ethics Committee (REC) and authorization from the health center’s management where the study will be conducted. This applies to any study using human specimens or data for evaluating an IVD’s performance, ensuring ethical considerations (informed consent, data protection, etc.) are addressed early.
When you need authorization
Interventional clinical performance studies and other studies involving risks require AEMPS authorization before first participant. Ethics approval remains mandatory.
What sponsors must prepare
- Spanish protocol (CPSP), Investigator’s Brochure, and informed consent.
- Insurance/indemnity for participants and a clear liability framework. The decree explicitly requires compensation for damages and defines the liability regime for sponsors. Sponsors should budget for a clinical trial insurance policy and follow the decree’s rules on coverage minimums and conditions (similar to drug trial insurance requirements in Spain).
- Monitoring, data management, and safety reporting plans aligned with IVDR. Upon study completion, results (whether positive, negative, or inconclusive) should be documented and may need to be reported in the public database or to AEMPS.
Studies with CE-marked devices
If the study adds invasive or burdensome procedures or goes outside intended use, sponsors should request authorization and notify AEMPS.
Action for sponsors: Build a Spain-ready dossier, confirm insurance, and align timelines with AEMPS and ethics reviews.
Vigilance and Market Control
The Spanish IVD Regulation 2025 reinforces vigilance. Manufacturers must report serious incidents and FSCAs to AEMPS. Healthcare professionals and institutions should also report incidents. Authorities will coordinate inspections and market control actions.
For instance, if an IVD test yields false results that lead to patient harm, the manufacturer has to notify AEMPS and submit a Spanish-language safety notice so that users in Spain can be adequately informed. This ensures critical safety information is effectively communicated and mitigated in the local context.
The decree emphasizes that healthcare professionals, health institutions, and even patients/users have a responsibility to report any suspected serious incidents to AEMPS. Spain is thus bolstering a culture of vigilance: a lab that encounters a device malfunction or a clinician who notices a pattern of erroneous results should alert the authorities. The more comprehensive the reporting, the better AEMPS can intervene to prevent harm.
Action: Maintain robust PMS plans, trend analysis, Spanish FSNs, and clear internal reporting lines. Hospitals should assign a vigilance lead and train teams.
Self-Test Access and Pharmacy Channels
Notably, the new rules remove the prescription requirement for at-home self-testing kits (e.g. self-tests for glucose, pregnancy, COVID-19, etc.), making them more accessible. However, even without needing a prescription, these self-diagnostic products can only be sold through pharmacies (in-store or via an official pharmacy website) to ensure proper guidance on use. High-risk tests or those used for critical decisions may still require a prescription or professional administration.
Action: Manufacturers should confirm packaging, leaflets, and e-commerce pharmacy guidance in Spanish.
Transitional Timelines You Should Track
- Entry into force: The decree takes effect after BOE publication.
- Licensing: Existing third-party manufacturers have up to one year to obtain the new operating license.
- Marketing register: Notification duties start when the register goes live.
- In-house devices: Spain applies the IVDR timelines. Labs must meet Article 5(5) conditions and ISO 15189 by the dates set in the transitional provisions and related guidance.
- Legacy devices: Spain honors the IVDR transition for legacy IVDs and preserves specific old-rule processes until systems fully switch over.
Action: Put a dated compliance tracker in place for licensing, Article 5(5), ISO 15189, registry readiness, and vigilance.
Implications by Stakeholder
IVD manufacturers
- Secure or update operating licenses.
- Localize labels/IFU into Spanish.
- Prepare marketing register data.
- Strengthen PMS and vigilance interfaces with AEMPS.
Sponsors
- Plan authorization for risk-involving performance studies.
- Build Spain-ready dossiers and insurance.
- Prepare Spanish IB, consent forms, and patient materials. Note: AEMPS may allow an english version of the IB if no objection is raised by the Ethics Committee.
Hospital and private labs
- Confirm Article 5(5) eligibility and prepare technical documentation for the in-house test.
- Achieve ISO 15189 for manufacturing scope.
- Notify AEMPS and assign the in-house responsible person.
- Update genetic testing consent and counseling SOPs.
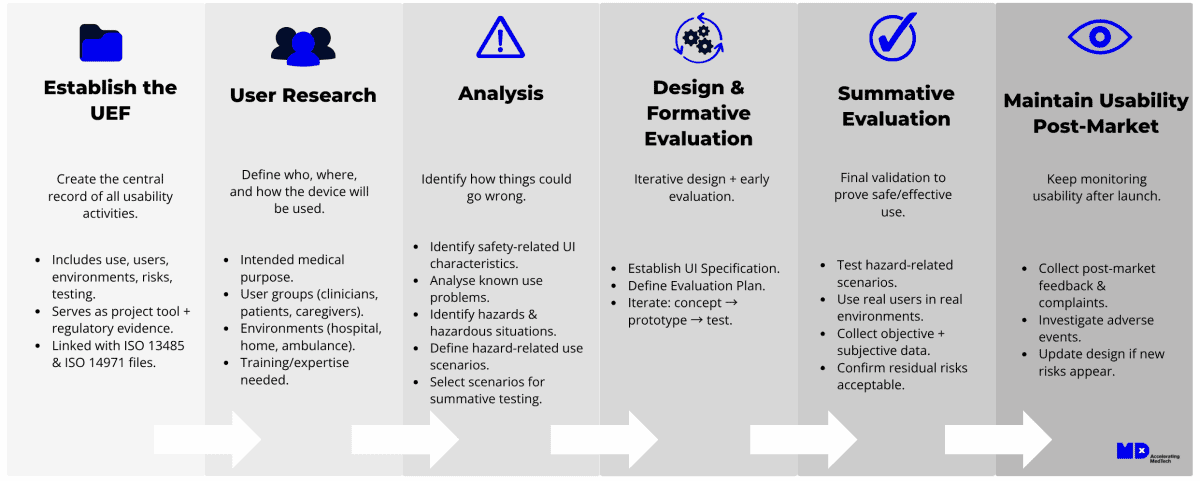
How MDx CRO Helps You Execute
Regulatory strategy and submissions
We align IVDR with the Spanish IVD Regulation 2025 and prepare AEMPS submissions (licenses, notifications, marketing register onboarding when live).
ISO 15189 and Article 5(5)
We run gap assessments, build SOPs, and guide labs to ISO 15189 accreditation for in-house manufacture. We prepare the Article 5(5) declaration and AEMPS notification package.
Performance studies
We plan and manage interventional and risk-involving performance studies in Spain. We handle AEMPS authorization, ethics submissions, monitoring, and safety reporting. MDx can also act your IVD performance study legal representative in the EU.
Vigilance and PMS
We design Spanish-compliant PMS frameworks, incident workflows, and FSNs. We help you interface with AEMPS and prepare for inspections.